Medical Plan Selections
Countdown to Open Enrollment!
Quick Nav Links
MEDICAL PLANS
Your Choice
There are three unique medical plan options, but each plan includes a choice of the
- National PPO - a comprehensive network throughout the country.
- High Performance Network (HPN) - a much narrower selection of providers who charge less for their services and agree to a higher level of managed care from Blue Cross Blue Shield of Arizona
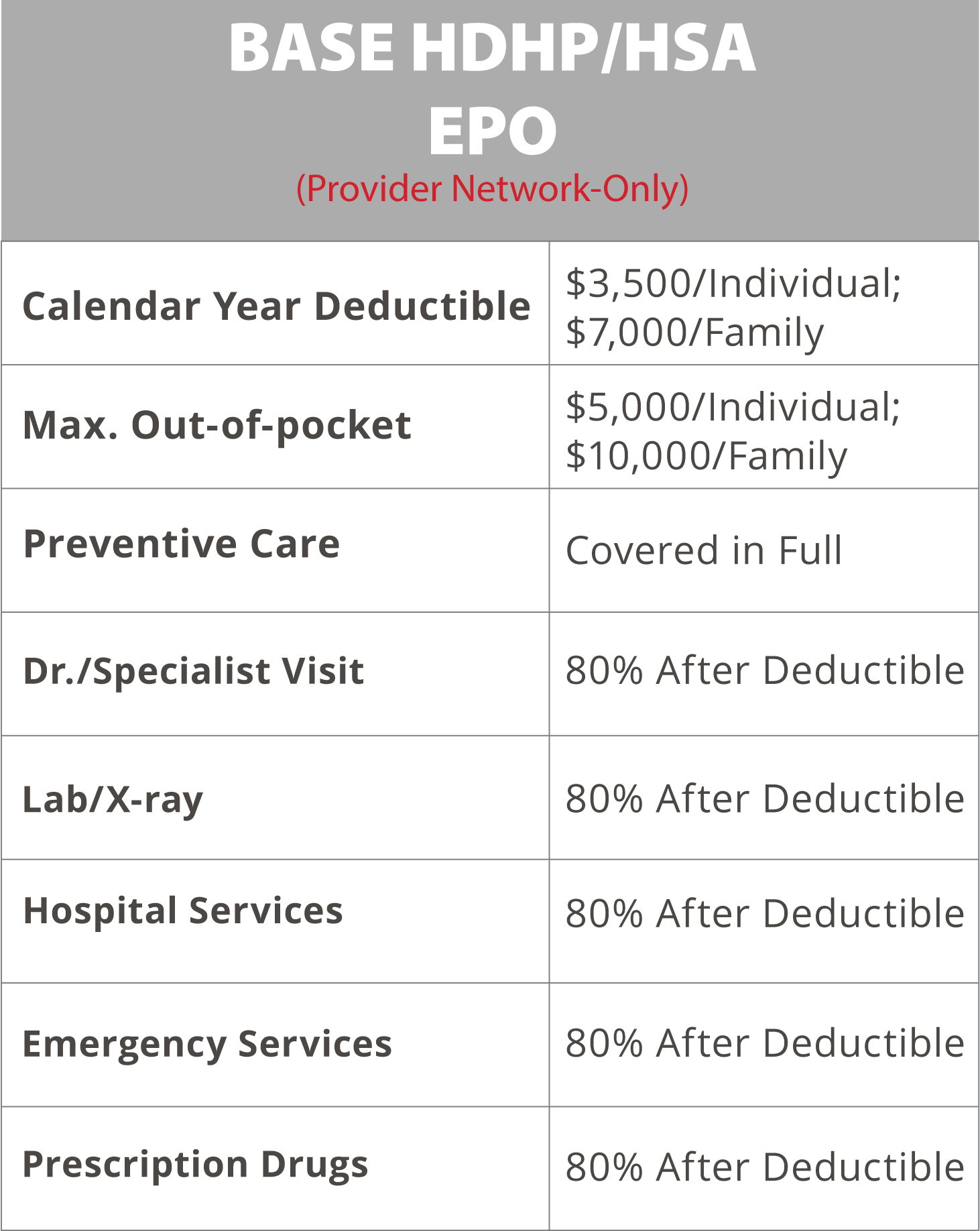
The BASE HDHP/HSA plan is an Exclusive Provider Organization plan (EPO). This means there is no "out-of-network" coverage. All care must be rendered within the EPO network.
As an HDHP plan, all charges apply as an out-of-pocket expense until the deductible is satisfied. The exception would be Preventive Care, which is covered at 100%
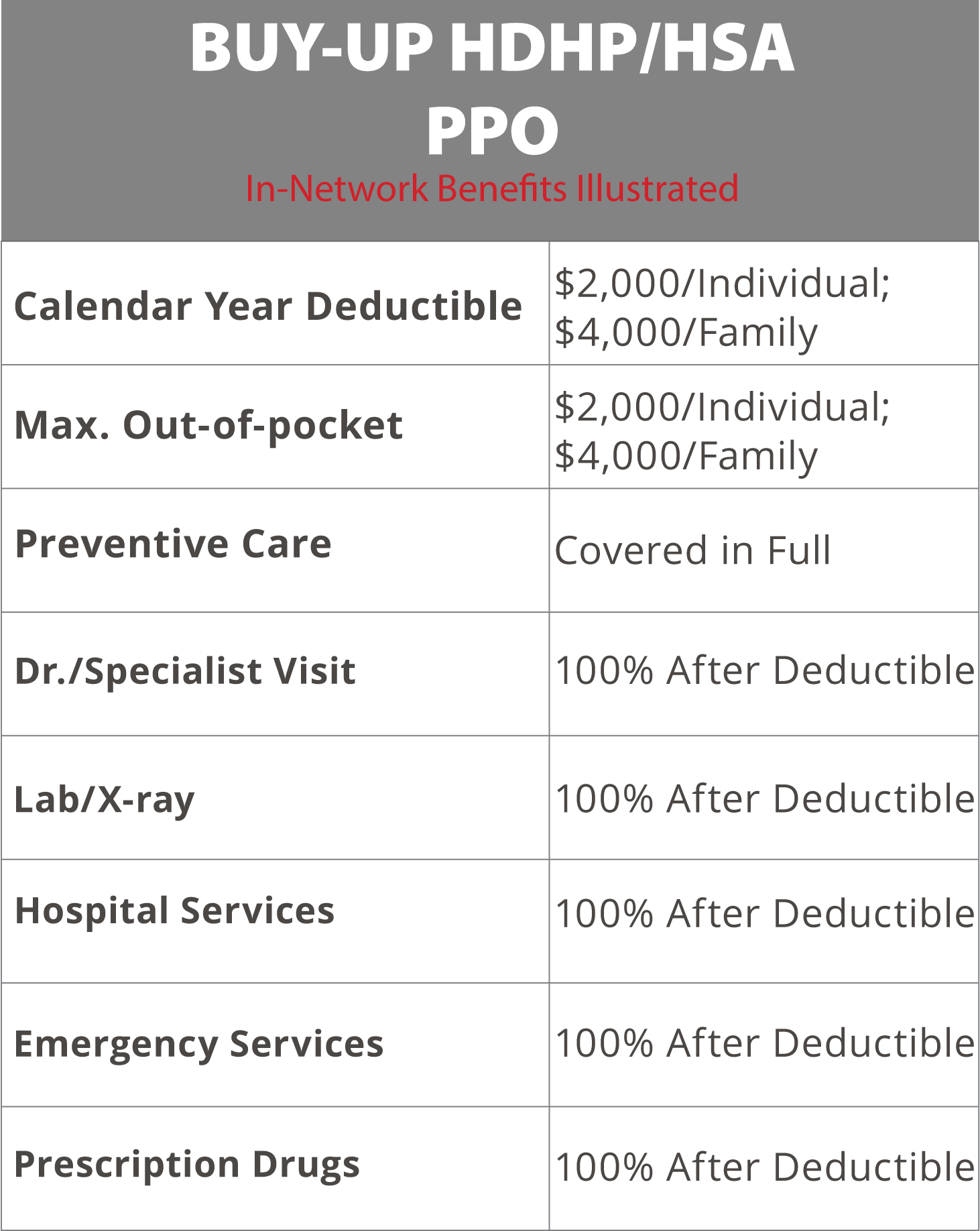
The BUY UP HDHP/HSA plan is Preferred Provider Organization plan (PPO). This means the plan does allow "out-of-network" coverage. Providers not within the network may "balance bill" for charges not covered by the plan.
As an HDHP plan, all charges apply as an out-of-pocket expense until the deductible is satisfied. The exception would be Preventive Care, which is covered at 100%
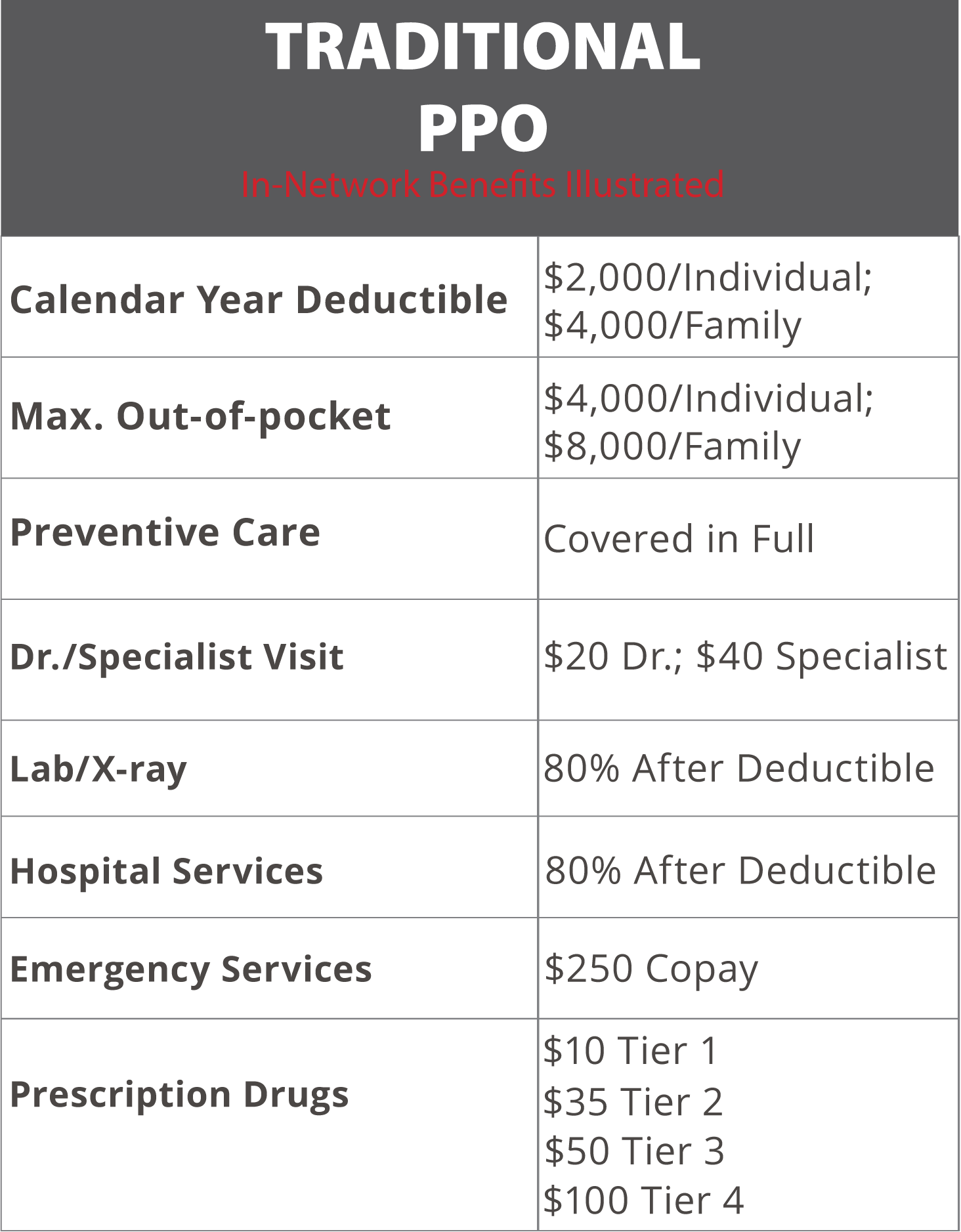
The PPO plan is Preferred Provider Organization plan (PPO). This means the plan does allow "out-of-network" coverage. Providers not within the network may "balance bill" for charges not covered by the plan.
As a PPO, the plan features copayments, lower deductible, and coinsurance. So some care - mostly outpatient, ambulatory services - are covered after a relatively low copay.
The above illustrations are intentionally brief for easy and quick comparison. They are not intended to represent the complete benefit descriptions of the plans shown. Please refer to actual plan documentation for a complete explanation of benefits and exclusions.
Premium Subsidy
ABC Company provides an additional medical premium subsidy for all benefits-eligible employees who earn an annual base salary under $50,000. Annual base salary for hourly employees is calculated by multiplying your hourly rate by 2,080 hours per year (overtime earnings are not included in the calculation). You must be enrolled in one of ABC Company’s medical plans to receive the subsidy.
The subsidy is provided through lower medical premium rates deducted from each paycheck while you are enrolled in
a medical plan.
The premium rates shown in this site in the “<$50k Base Salary” columns show you what your cost will be after the subsidy is applied.
If the medical premium for the plan you elect is less than the subsidy, your premium cost will be $0 and you will not receive the difference. If your base salary is increased above $50,000, the subsidy will stop in the first paycheck reflecting your new pay rate.
| Enrollment | Subsidy Per Month |
|---|---|
| Employee Only | $20 |
| Employee + Spouse | $50 |
| Employee + Child(ren) | $50 |
| Employee + Family | $75 |
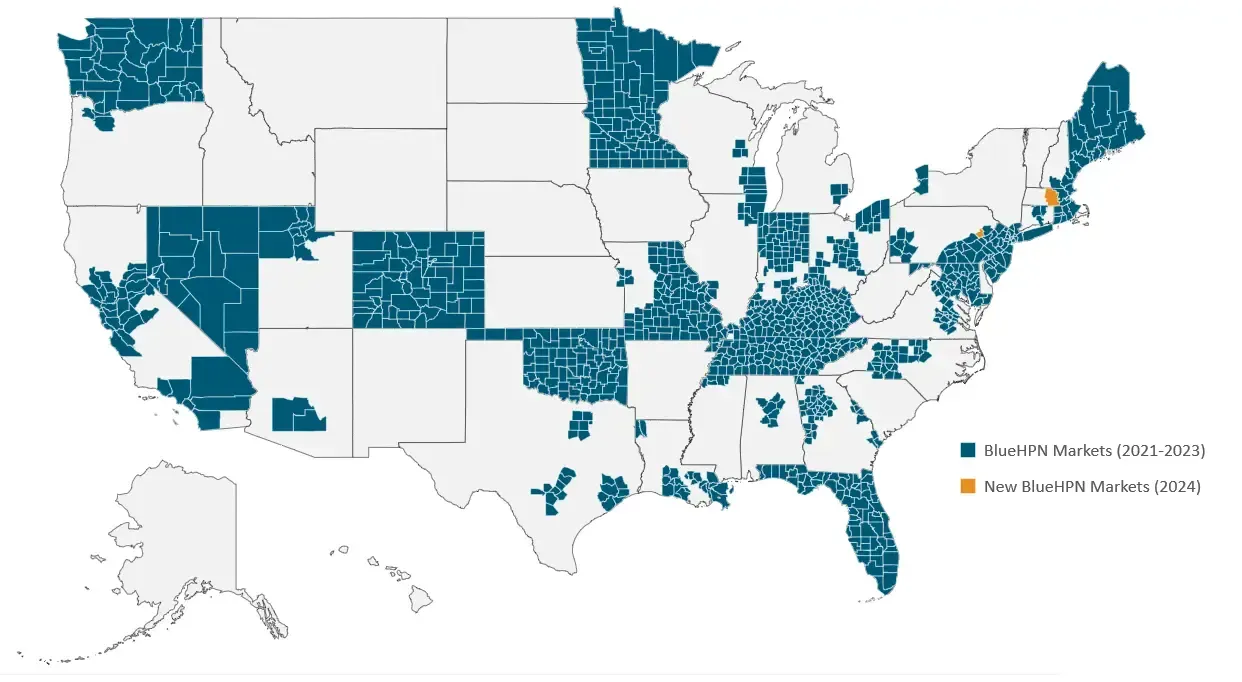
High Performance Network
What Is the HPN?
Notice that there are three separate medical plan selections, but two choices for each plan. You can either select the National PPO plan, or the High Performance Network plan (HPN). Here are the two important distinctions between these selections:
Where Are HPN Providers?
Available in 65+ major metro areas across the U.S., BlueHPN includes all provider types from primary care physicians to specialists and hospitals. You and your employees will have the flexibility to visit any provider in the BlueHPN network without a referral. Plus, you’ll have access to emergency care and telehealth services anywhere.
Be sure to check if certain providers are in the BlueHPN network, as out-of-network services are not covered.
Is the HPN Right For You?
Sure, the HPN network option is less expensive out of your paycheck, but is is right for you?
The HPN is a narrower network. Meaning fewer providers - and sometimes no providers. It depends on where you live if there are HPN providers you can access.
HPN FAQs
Here is a good place to start to learn how to determine if the HPN network is the best fit for you and your family.
Want More Detail?
Here, you can get a more detailed explaination of the HPN, how it works, and mechanisms and resources that help contain health care costs.
Eligibility
Eligible Employees:
You may enroll in the Employee Benefits Program if you are a full-time employee who is actively working a minimum of 30 hours per week.
Eligible Dependents:
If you are eligible for our benefits, then your dependents are too. In general, eligible dependents include:
- Your Legal Spouse
- Civil Union - Colorado
- Common Law Spouse in Colorado, Idaho
- Registered Domestic Partner in California, Nevada, Oregon and Washington and children up to age 26
- If your child is mentally or physically disabled, coverage may continue beyond age 26 once proof of the ongoing disability is provided
- Children may include natural, adopted, stepchildren and children obtained through court-appointed legal guardianship, as well as children of state-registered domestic partners
When Coverage Begins:
Newly hired employees and dependents will be eligible on the first day of the month following 30 days of employment. All elections are in effect for the entire plan year and can only be changed during Open Enrollment unless you experience a family status event.
Family Status Change:
- A qualifying life event is a change in your personal life that may impact your eligibility or dependent’s eligibility for benefits. Examples of some family status changes include:
- Change of Legal Marital Status (i.e. marriage, divorce, death of spouse, legal separation)
- Change in Number of Dependents (i.e. birth, adoption, death of dependent, ineligibility due to age)
- Change in Employment or Job Status (spouse loses job, etc.)
- If such a change occurs, you must make the changes to your benefits within 30 days of the event date; 60 days for loss of Medicaid or state child health plan. Documentation may be required to verify your change of status. Failure to request a change of status within 30 days of the event or 60 days for loss of Medicaid or state child health plan coverage, may result in your having to wait until the next open enrollment period to make your change. Please contact HR to make these changes.

Changes in Elections
- Qualifying life events are specific life events that allow individuals to make changes to their health insurance coverage outside of the regular enrollment period. These events include:
- Marriage or divorce
- Birth or adoption of a child
- Loss of other health coverage
- Change in residence that affects health plan options
- Change in employment status
- Turning 26 and aging out of a parent's health plan
- Qualifying Life Events allow you to enroll in a new health plan, add or remove dependents from your coverage, or make other changes to your health insurance outside of the regular enrollment period.
When?
You must notify Human Resources within 30-days of your Qualifying Life Event to be eligible to make changes during the plan year.
How?
If you have had a Qualifying life event, you must notify Human resources of your event and that you would like to make changes to your benefit plan elections.